283 St Rose Ave
Windsor, ON N8S 1X1

Causes of Plantar Warts

Plantar warts are noncancerous growths caused by the human papillomavirus, or HPV, infecting the outer layer of skin on the soles of the feet. They often appear as small, grainy lesions with black dots embedded within them, causing discomfort or pain, especially when walking or standing. Those individuals with diabetes or compromised immune systems should be particularly watchful of such growths. These warts are contagious and can spread through direct contact with infected surfaces or skin. Treatment options can include salicylic acid to prescription strength treatments such as cryotherapy, laser therapy, or surgical removal. If you have a plantar wart that causes persistent pain, changes in appearance, or interferes with walking, it is suggested that you seek podiatric attention.
Plantar warts can be very uncomfortable. If you need your feet checked, contact the practitioners from Foot Care Institute. Our practitioners will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Windsor, ON . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Are Plantar Warts?
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
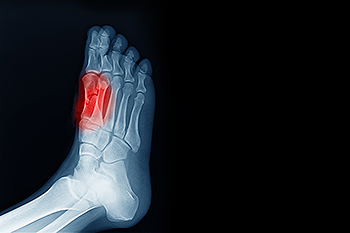
Causes of Foot Stress Fractures

Stress fractures typically occur when there is a rapid increase in activity level or time spent on your feet. Your bones are resilient, constantly adapting to changes through a process called remodeling. However, when this adaptation is rushed, such as with sudden increases in activity, the balance between bone destruction and rebuilding is disturbed. This leaves your bones fragile and susceptible to stress fractures. Conditions like osteoporosis as well as high-impact sports may increase the risk of stress fractures. Foot structure variations like high or flat arches and wearing inadequate footwear can also contribute to heightened stress fracture risk. Symptoms of foot stress fractures include swelling, bruising, tenderness, and activity-related pain that diminishes with rest. Ignoring a foot stress fracture can make the injury worse and potentially lead to more severe consequences. If you believe you may have a foot stress fracture, it is suggested that you schedule an appointment with a podiatrist.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact the practitioners from Foot Care Institute. Our practitioners can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Windsor, ON . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
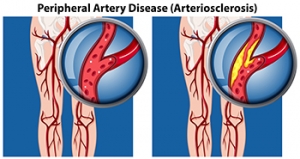
Symptoms and Causes of Peripheral Artery Disease
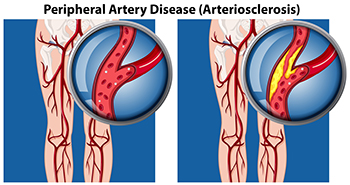
Peripheral artery disease, or PAD, is a common condition characterized by a buildup of fatty deposits in the arteries, resulting in restricted blood flow to the muscles in the lower legs and feet. A particular symptom of PAD is called intermittent claudication, which is a pain, cramp, or sense of fatigue in the leg muscles when you walk or exercise. Other symptoms are hair loss on the legs and feet, numbness or weakness, and slow-growing toenails. Leg ulcers, skin color changes, and shiny skin are other signs. PAD is primarily caused by atherosclerosis, where fatty deposits accumulate within arterial walls, narrowing the vessels. Contributing factors to peripheral artery disease include smoking, diabetes, high blood pressure, high cholesterol, and aging. Seeking help from a podiatrist is essential for an accurate diagnosis through physical examination and tests like the ankle brachial pressure index, or ABPI. Treatment involves lifestyle modifications, such as regular exercise, smoking cessation, and maintaining a healthy diet. In severe cases, surgical intervention may be needed to improve blood flow and alleviate symptoms. For help in determining whether you have peripheral artery disease that is affecting your foot health, it is suggested that you schedule an appointment with a podiatrist.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with the practitioners from Foot Care Institute. Our practitioners will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Windsor, ON . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Big Toe Pain and Sesamoiditis
 Sesamoiditis is an inflammation of the sesamoid bones, two tiny bones beneath the big toe joint. These bones are embedded within the tendons that allow the big toe to move. Sesamoiditis typically occurs from overuse or repetitive stress, making it common among athletes and dancers. Symptoms of sesamoiditis include pain in the ball of the foot, especially when walking or running, and swelling or bruising in the area around the big toe. The pain might worsen when the big toe is used, such as when pushing off to jump or take a step. Bending and straightening the big toe may also become difficult. If you have a painful big toe or ball of the foot, it is suggested that you consult a podiatrist for a proper diagnosis and treatment plan.
Sesamoiditis is an inflammation of the sesamoid bones, two tiny bones beneath the big toe joint. These bones are embedded within the tendons that allow the big toe to move. Sesamoiditis typically occurs from overuse or repetitive stress, making it common among athletes and dancers. Symptoms of sesamoiditis include pain in the ball of the foot, especially when walking or running, and swelling or bruising in the area around the big toe. The pain might worsen when the big toe is used, such as when pushing off to jump or take a step. Bending and straightening the big toe may also become difficult. If you have a painful big toe or ball of the foot, it is suggested that you consult a podiatrist for a proper diagnosis and treatment plan.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact the practitioners of Foot Care Institute. Our practitioners will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Windsor, ON . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscle. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high arched feet, flat feet, or runners who run on the ball of their foot are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high arched feet to relieve pressure off the bones. In some cases the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
Causes of Foot Tendon Pain

Foot tendon pain, often termed tendonitis, can arise from various causes. Tendons are essential for foot function because they connect muscles to the foot's many bones and support daily activities like walking and running. Common causes of foot tendon injury include wearing ill-fitting footwear, sudden foot movements, repetitive stress from activities like sports, and trauma. Structural issues, such as flat feet or high arches, can predispose individuals to tendon problems. Age-related degeneration and medical conditions, like diabetes and rheumatoid arthritis, are other contributing factors to foot tendon pain. Obesity increases the risk of tendonitis due to increased pressure on the feet. Also, overuse, weak muscles, and loose ligaments can contribute. Understanding these factors helps individuals to take proactive steps to safeguard their foot health. If you are experiencing persistent foot tendon pain or discomfort, it is suggested that you schedule an appointment with a podiatrist for a comprehensive evaluation and diagnosis, followed by a personalized treatment plan.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with the practitioners from Foot Care Institute. Our practitioners will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Windsor, ON . We offer the newest diagnostic and treatment technologies for all your foot care needs.